03/07/2026
PODIATRISTS IN THE NEWS
Tread Mill is Best Alternative for Unsteady Walkers: MD Podiatrist
Walking is rightly hailed as an accessible and effective type of exercise, but that doesn’t mean everyone finds walking easy to do. For instance, walking outdoors can be scary if you’re unsteady on your feet. That’s where a treadmill can come into its own, according to Mikel Daniels, DPM, the president and chief medical officer at WeTreatFeet Podiatry.
 |
Dr. Mikel Daniels |
Dr. Daniels told me that the treadmill is clearly the better place to start walking for those with neuropathy who can’t reliably feel the ground, patients with a history of ankle sprains or poor balance, and people recovering from surgery who need a predictable footing and easy access to a handrail. “In these cases, the smooth belt, climate control, and the ability to stop instantly make treadmill walking safer and more sustainable,” he says.
Source: Lou Mudge, Fit and Well [3/5/26]
03/05/2026
PODIATRISTS IN THE NEWS
IL Podiatrist Provides a Six-Step Plan to Treat Onychomycosis
According to John M. Sigle, DPM, “Achieving clear nails requires a multi-faceted, customized approach.” If you want healthy nails by summer, here is the proven six-step plan that offers effective results: 1) Get an accurate diagnosis 2) Prepare the nails for treatment 3) Use laser therapy 4) Restore nails with Keryflex 5) Use science-based topicals and 6) Sanitize footwear.
 |
Dr. John Sigle |
"Managing toenail fungus is a marathon, not a sprint. Success depends on a correct diagnosis and a multi-faceted, customized approach using the best products, medications, and state-of-the-art technology to combat the condition. While laser treatments are often an out-of-pocket expense, some insurance carriers are beginning to provide coverage. Now is the ideal time to start treatment so your feet are healthy and ready for sandal season," says Dr. Sigle.
Source: Illinois Times
03/04/2026
PODIATRISTS IN THE NEWS
PA Podiatrist Discusses Causes of Bunions
A bunion is a bony bump that sticks out from the side of your foot at the base of the big toe. The word bunion comes from the Greek word for turnip – perhaps because a bunion can look swollen and reddish. “The common wisdom is that women get bunions because they spend too much time in narrow-toed high heels,” says Brian Stahl, DPM, a podiatrist and foot and ankle surgeon with LVPG Podiatry–Hecktown Oaks.
 |
Dr Brian Stahl |
“Tight shoes can certainly be a contributing factor,” he says, “but bunions can be caused by anything that puts extra pressure on your big toe joint, such as the way you walk, standing for a long time, and even some health conditions.” Heredity or previous foot injuries also can be a factor, Dr. Stahl says.
Source: Paul Wirth, Lehigh Valley Health Network [3/3/26]
03/02/2026
PODIATRISTS IN THE NEWS - PART 2
TX Podiatrist Advocates for Early Foot & Wound Care Awareness
Hope Jacoby, DPM of the Dallas-Fort Worth area is urging patients to take foot pain and lower extremity wounds seriously before small issues become life-altering complications. "Foot pain is often dismissed as minor," says Dr. Jacoby. "But the feet carry the entire body. When something is wrong, it affects balance, mobility, and overall health."
 |
Dr. Hope Jacoby |
Chronic wounds affect an estimated 6.5 million patients nationwide and cost the U.S. healthcare system billions annually. She emphasizes that early symptoms - such as numbness, slow-healing sores, swelling, or persistent foot pain - should never be ignored. "By the time some patients seek treatment, the condition has progressed significantly," she says. "The earlier we intervene, the better the outcome."
Source: Access Newswire [2/27/26]
03/02/2026
PODIATRISTS IN THE NEWS - PART 1
People Take Their Feet for Granted: PA Podiatrist
“We really do take our feet for granted, and oftentimes it can be very hard to find time to come into the doctor. Ultimately, these small problems can lead to further issues like joint pain or arthritis,” says Kevin Wotring, DPM, a surgical podiatrist at St. Luke's University Health Network. “The most common ones are going to be plantar fasciitis, bunions, nail disorders, as well as ankle sprains.”
 |
Dr. Kevin Wotring |
“We always try to exhaust our conservative options. But for some things like a trauma, like an acute tendon rupture or for severe bunions deformities, surgery is indicated. Every surgical procedure is going to have different recovery process, but we like to walk patients through what the surgery is going to encompass as well as every single step along the way regarding getting them back on their feet,” says Dr. Wotring.
Source: Liz Keptner, WFMZ [2/26/27]
02/26/2026
PODIATRISTS IN THE NEWS
Exercise Today – for a Healthy Tomorrow: MD Podiatrist
Mikel Daniels, DPM, President and Chief Medical Officer at WeTreatFeet Podiatry, Baltimore, USA, says, As we age, we all enter the ‘use it or lose it’ phase of life. If you don’t use it now, you won’t be able to do it later.” A strong sense of balance is the foundation of independence in later life. U.S. Centers for Disease Control and Prevention (CDC) estimates 1 in 4 older adults has a fall each year - with 10% of those falls resulting in a fracture. Dr. Daniels says, “Balance training can keep you upright and independent.”
 |
Dr. Mikel Daniels |
“When weightlifting, use heavier lifts with fewer reps. But go slow - use light weights and perfect your form first, then build up gradually. Stick to 10-30 minutes twice weekly for several months to turn back the clock on strength loss,” says Dr. Daniels. “Sneak 15-30 seconds stretches as ‘movement snacks’ during TV breaks or while the kettle boils. Breaking them up is way more doable than one big session,” he adds. Finally, “post-session, grab a quick protein snack like milk, nuts, or hummus on crackers. These allow you to lock in gains. But be careful if kidneys or diabetes are factors for you.”
Source: Lawrence Higgins, Patient [2/15/26]
02/25/2026
PODIATRISTS IN THE NEWS
CA Podiatrist Discusses the Benefits of Wearing Shoes Indoors
If you already deal with foot pain, then it’s particularly important to wear indoor shoes, says Bobby Pourziaee, DPM, “The High Heel Doctor” and a board-certified foot and ankle surgeon. “Supportive footwear reduces repetitive strain on the plantar fascia, distributes pressure evenly, minimizes arch collapse, and decreases muscle overwork,” Dr. Pourziaee says.
 |
Dr. Bobby Pourziaee |
“Those with plantar fasciitis, flat feet, high arches, or heel pain often benefit from avoiding prolonged barefoot time indoors,” he says. But you want to make sure that you’re actually choosing the right kind of indoor footwear. And how do you do that? “Supportive house shoes should have structured arch support, a stable heel counter, cushioned but not overly soft midsoles, and a firm outsole.”
Source: Melissa Matthews, Real Simple [2/17/26]
02/25/2026
INTERNATIONAL PODIATRISTS IN THE NEWS
UK Patient Hails Podiatry Team for Getting Him Walking Again
A North East patient has credited NHS advice with helping him get back on his feet and rediscover the joy of walking. Joseph Telford of Eaglescliffe has praised the podiatry team at University Hospitals Tees after their treatment and guidance not only healed a foot problem but also encouraged a more active lifestyle.
 |
The podiatry team at University Hospitals Tees |
Mr. Telford, 75, was referred to the service after developing a painful toe ulcer that turned black following an injury. Andrea Deiac, a podiatrist, said: "It’s fantastic to see that Mr. Telford has made such great progress – thanks to both the expert advice of the team but also to his dedication in following this advice and support.
Source: Gavin Engelbrecht, Yahoo! News {2/22/26]
02/24/2026
PODIATRISTS IN THE NEWS
MA Podiatrist Discusses the Use of PRP Therapy
Platelet-rich plasma therapy (PRP) aims—and claims—to supercharge the body’s natural recovery processes, whether needed for a strained muscle or a scalp sparse from hair loss. With an injury, the platelet is what “creates a clot and sends out growth factors and a whole host of other chemicals to start this very beautiful and predictable chain of events—the inflammatory cycle itself,” explains Michelle Morse, DPM, a foot and ankle surgeon in Massachusetts. “So the idea [with PRP] is: Can we make that very potent, our body’s own natural way of healing?”
 |
Dr. Michelle Morse |
“Prior to me knowing much about PRP, I just viewed it as an expensive Hail Mary right before you go to surgery,” says Dr. Morse, a foot and ankle surgeon. But then she joined a new practice and began to integrate PRP into her offerings. “Now I am a full-fledged believer in our body’s own power to heal.” Dr. Morse says clinicians should be injecting with the guidance of an ultrasound “so you know exactly where you’re putting it.”
Source: Anna Medaris, Women's Health [2/18/26]
02/24/2026
INTERNATIONAL PODIATRISTS IN THE NEWS
Aussie Podiatrist Discusses Women's Foot Health
For women, being pregnant can bring more change to the feet. “Not only do you get the effects of relaxin hormone, which enables you to give birth,” says Hylton Menz, Professor of Podiatry at La Trobe University’s School of Allied health, Human Services and Sport “that actually acts on all the different levels in your body, including your feet. There is a tendency for your feet to spread, so to become a bit wider and for the arch to get lower as pregnancy develops.”
 |
Dr. Hylton Menz |
At any age, podiatrists say, give your nails a break from nail polish from time to time: “It does actually mask things like, if you’ve got say, onychomycosis, which is like a fungal infection of your nails,” says Dr. Menz. Speaking of which, opt to keep your cuticles intact; they function as a protective seal, just as your nails protect your digits.
Source: Madeleine Heffernan, The Sydney Morning Herald [2/22/26]
02/23/2026
PODIATRISTS IN THE NEWS
NYC Health + Hospitals/Harlem Opens State-of-the-Art Ortho & Podiatry Clinic
NYC Health + Hospitals/Harlem today announced the opening of its new $10 million Orthopedic and Podiatry Clinic, designed specifically to meet the complex needs of orthopedic and podiatry patients, expanding access to coordinated, high-quality musculoskeletal care in the Harlem community.
 |
NYC Health + Hospitals/Harlem State-of-the-Art Orthopedic and Podiatry Clinic |
The redesigned space was thoughtfully built with patient mobility, safety, and comfort at the forefront. Features include 9 all-new exam rooms equipped with high-low exam tables, including bariatric exam tables, ergonomic provider workstations within exam rooms, and a waiting area with higher-seated chairs to allow patients to sit and stand comfortably.
02/19/2026
PODIATRISTS IN THE NEWS
VA Podiatrist Assists Monks on Thousand Mile Walk
David Weiss, DPM was recently asked to provide podiatric medical support to the group of monks who undertook the extraordinary journey of walking from Texas to Washington, DC. Covering hundreds of miles over variable terrain with limited recovery time created a predictable cascade of lower extremity pathology: friction blisters with maceration risk, plantar fascial strain, Achilles tendinitis, forefoot capsulitis, and early metatarsal stress reactions. The cumulative load without structured rest cycles was the defining variable. Minor mechanical inefficiencies, when repeated daily, amplified quickly. "It was a humbling, amazing experience to witness both the physiologic limits of the lower extremity and the discipline required to push beyond them," said Dr. Weiss.
 |
Dr. David Weiss (far right) with monk and two physicians. |
Management centered on prevention and maintaining forward progress — advanced blister care with selective drainage and hydrocolloid protection, strategic off-loading and taping, orthotic modifications rather than full device replacement, footwear counseling, and early identification of stress-related symptoms before progression. "The experience reinforced a simple truth we all appreciate: control shear and you prevent most complications. In high-mileage endeavors, success often hinges not on dramatic intervention, but on millimeters of padding, timely biomechanical support, and early clinical judgment," said Weiss.
02/18/2026
PODIATRISTS IN THE NEWS
MA Podiatrist Discusses Home Treatment of Plantar Fasciitis
Plantar fasciitis afflicts around one in 10 people at some point in their lives. It can be chronic or acute, and in either case, it’s painful and frustrating. And in serious cases, it can be "extremely debilitating," according to foot and ankle surgeon Michelle Morse, DPM. "A splint worn while you sit or sleep keeps your foot gently flexed, which stretches the plantar fascia tissue and Achilles tendon. This helps prevent the tissue from tightening up, reducing heel pain. I instruct them to use it between 30 to 60 minutes a day with a pillow under the heel so the knee can relax down,” says Morse. And for patients with extreme morning time pain, she recommends using the splint overnight “to keep all the tissue stretched out."
 |
Dr. Michelle Morse |
According to Dr. Morse, the first massaging you do to help treat plantar fasciitis should actually begin before you even get out of bed in the morning. After sleeping, the tissues are cold and tight. A quick stretch and calf massage prior to getting out of bed can make the first steps of the day much less painful. And a more involved massage and ice treatment can reduce symptoms and promote healing.
Source: Steven John, Forbes [2/13/26]
02/16/2026
PODIATRISTS IN THE NEWS
Morning Exercises Strengthen Leg Muscles Faster After 55: MD Podiatrist
"When my older patients get into a habit of doing a simple leg routine early in the day, I see the following:” explains Mikel Daniels, DPM, board-certified podiatrist with WeTreatFeet Podiatry. "First and foremost, morning exercise sets a solid tone for the entire day. If you start your day with a little focused strength, you are far more likely to stand more, walk more, and use those muscles throughout the day."
 |
Dr. Mikel Daniels |
"Second, performing a productive morning sweat session helps alleviate stiffness. Overnight, joints get stiff, circulation slows, and many people over 55 tell me their first 10 minutes out of bed feel like they’re walking in concrete (I am almost there and trust me it is true)." Dr. Daniels notes. "Gentle leg work in the morning pumps blood through the muscles, lubricates the joints, and reduces that stiffness window." In addition, working out in the morning has the power to boost your mood. Resistance exercise in general is associated with improved energy, cognitive function, and mood. If you do it early on in the day, those benefits carry through.
Source: Alexa Mellardo, Eat This, Not That! [2/13/26]
02/13/2026
PODIATRISTS IN THE NEWS - PART 2
NY Podiatrist Discusses How Hormonal Changes Affect Older Women's Feet
According to Amnon Barnea, DPM, Founder of Walk NYC Podiatry, "Hormonal changes – especially the drop in estrogen, directly affect the tissues that keep the foot stable, cushioned, and pain-free. Estrogen supports collagen, joint cartilage, bone density, nerve sensitivity, and the plantar fat pads that provide natural shock absorption. As levels decline, support structures lose strength, the fat pads under the heel and forefoot thin, shock absorption decreases, arches can weaken, cartilage wears faster, bones become more prone to stress injury, and some women develop burning or hypersensitive feet."
 |
Dr. Amnon Barnea |
"Women can be proactive by staying active to preserve strength and circulation, maintaining a routine of stretching and strengthening, following a bone-healthy diet, and wearing shoes with solid structural support and cushioning. Most importantly, when alignment and stability begin to change, proper biomechanical support becomes essential to reduce strain and prevent many of the problems that commonly develop during this stage of life," says Dr. Barnea.
Source: Anne Akers, The Three Tomatoes [2/11/26]
02/13/2026
PODIATRISTS IN THE NEWS - PART 1
TX Podiatrist Extolls the Benefits of Walking 30 Minutes a Day
Walking 30 minutes per day can improve your physical endurance. This is when your heart and lungs become more efficient at supplying energy to your working muscles by using oxygen for fuel, says exercise physiologist Tamara Hew-Butler, DPM, PhD. Essentially, modest aerobic activity (like walking) can stimulate the growth of mitochondria, or the “powerhouses” of cells, Dr. Hew-Butler says. In turn, muscle tissues become more effective at using fat and oxygen for fuel, thereby making physical activity easier.
 |
Dr. Tamara Hew-Butler |
And if you already have type 2 diabetes? “Walking is an excellent way to lower elevated blood sugar levels,” Dr. Hew-Butler says. That’s because it stimulates working muscle tissue to transport glucose directly into the muscle cells, ultimately reducing its reliance on medications to do the job. Additionally, Dr. Hew-Butler says that research has found that exercise (such as walking 30 minutes per day) reduces anxiety and depression by increasing the brain’s production of mood-related neurotransmitters, including endorphins.
Source: Kirsten Nunez, Real Simple [2/11/26]
02/02/2026
PODIATRISTS IN THE NEWS
MD Podiatrist Discusses What to Look for in an Insole
When recommending insoles for nurses, teachers, hair stylists, warehouse workers, or runners, Mikel Daniels, DPM, president and chief medical officer at WeTreatFeet Podiatry, looks for three key features: a true heel cup, a stable arch, and enough cushioning to handle hard floors.
 |
Dr. Mikel Daniels |
A deep heel cradle stabilizes the foot and helps maintain proper alignment. Every runner moves differently, and high arches often need more flexible support. Heel-to-toe cushioning helps prevent common running injuries.
Source: Christopher Murray, Fox News [1/30/26]
01/31/2026
PODIATRISTS IN THE NEWS
MD Podiatrists Discuss Plantar Fasciitis
You should not wake up and dread taking your first step of the day. If you do, there’s a pretty good chance you have plantar fasciitis. “Feeling pain when you take your first step in the morning is a hallmark sign of plantar fasciitis,” says Priya Parthasarathy, DPM ,a podiatrist at the Foot & Ankle Specialists of the Mid-Atlantic. “Patients tend to ignore it because it usually goes away once you start moving, but it can advance to pain after activity, during activity, or all the time.”
 |
Drs. Priya Parthasarathy and Jacob Wynes |
If you address symptoms as soon as you feel them, plantar fasciitis is relatively easy to deal with — and conservative treatments like stretching, icing, and massaging work 90% of the time, says Jacob Wynes, DPM, a podiatric surgeon and an associate professor of foot and ankle surgery for the University of Maryland Medical System. If you suspect you have plantar fasciitis, first consult your podiatrist to rule out other issues, like nerve damage, stress fractures, bursas, and bone spurs.
Source: Zoe Malin, NBC News [1/29/26]
01/29/2026
HOSPITAL PODIATRISTS IN THE NEWS
CT Podiatrist Awarded the Physician Recognition Award at Greenwich Hospital
Lady Paula DeJesus, DPM has been awarded the Physician Recognition Award at Greenwich Hospital. Dr. DeJesus earned her podiatric medical degree at the Barry University School of Podiatric Medicine and completed her podiatric residency at Wyckoff Heights Medical Center in Brooklyn, NY.
 |
Dr. Lady Paula DeJesus |
Dr. DeJesus is a triple board-certified podiatrist with certifications in Podiatric Surgery, Podiatric Medicine, and Wound Care. Her clinical expertise focuses on complex foot surgeries, lower extremity wound management, foot infections, minimally invasive foot reconstruction, and non-surgical podiatric management.
Source: LinkedIn
01/28/2026
PODIATRISTS IN THE NEWS
NY Podiatrist Warns of Risks of Wearing Snow Boots
It’s important for every New Yorker to be cautious of the foot and ankle problems that can be caused or worsened by wearing snow boots,” Rock G. Positano, DPM, a podiatrist for the Hospital for Special Surgery, told The Post. “Since there are more risks than rewards with snow boots, these shoes certainly aren’t made for walking.” Positano noted that while snow boots appear “safe,” they offer little to no orthopedic support. “This leads to tendon and ligament overuse, which can cause painful injuries, especially when making long treks in the snow or in the rain,” he explained.
 |
Dr. Rock G. Positano |
“An influx of knee and back problems can also arise from the lack of support, mixed with the presence of underlying orthopedic problems.” In addition, Positano shared that snow boots are not as well insulated as we might assume, and this lack of protection can lead to skin issues such as frostbite and ulceration. “The likelihood of these can increase if you also have sensitive skin,” he added, “so making sure you have footwear that can handle harsh weather but accommodate any skin conditions is vital.”
Source: Reda Wigle, The New York Post [1/23/26]
01/27/2026
PODIATRISTS IN THE NEWS
NY Podiatrist Describes the Benefits of Insoles
While a good pair of shoes can take you far, when you're walking miles upon miles or standing all day, sometimes you need a little something more to keep your feet comfortable and pain-free. That's where insoles come in. “Insoles are absolutely everything for the stability and structure of our feet,” says Brad Schaeffer, DPM, a board-certified podiatrist and foot surgeon at Central Park SOLE.
 |
Dr. Brad Schaeffer |
“Our feet are our body's natural shock absorbers and stabilizers, so it is very important to get a good shoe/sandal and especially an insole. If you have the appropriate insole, you will feel supported and also feel comfortable throughout your activity and day,” Dr. Schaeffer suggests.
Source: Emma Stressman, Today [1/26/26]
01/23/2026
PODIATRISTS IN THE NEWS
SC Podiatrist Helps Monks During Nationwide 'Walk for Peace'
North Charleston podiatrist Jamelah Lemon Youmans, DPM and fellow Lowcountry physicians played a key role caring for Buddhist monks on a 2,300-mile 'Walk for Peace,' coordinating intensive medical support during their Columbia stop. The volunteer team treated blisters, dehydration, and fatigue, turning the visit into a powerful example of Charleston-area medical professionals rallying around compassion and community service.
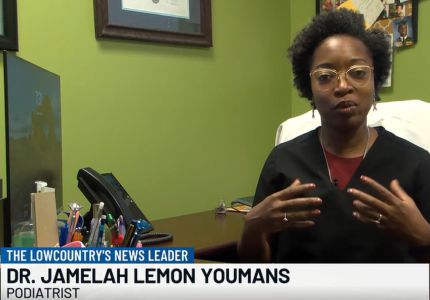 |
Dr. Jamelah Lemon Youmans |
For two days, Drs. Boston, Sellers, Bryant, and Lemon Youmans were all part of the team administering IV fluids to the monks, checking their vitals, caring for their blisters, calluses, and other injuries. “It was a lot of kind of pandemonium before the monks arrived, but it was like once they came into the room, there was kind of this sense of calm and peace and we all just kind of sprang into action,” Dr. Lemon Youmans said.
Source:: Shelbey Roberts, WCSC [1/21/26]
01/23/2026
PODIATRISTS IN THE NEWS
Modern Lifestyles a Major Contributor to Cancer: NY Podiatrist
Board certified podiatrist Kordai DeCoteau, DPM — founder and CEO of Sisters on the Vineyard, a health and wellness advocacy group — spoke from the perspective of a cancer survivor. According to her, our modern lifestyle isn’t helping at all. “I was tested for genes out of the wazoo, and was negative,” Dr. Kordai said of her stage 2 cancer diagnosis. “I did not have a child before 35, I was overweight, I was stressed out — as most women are who are working and taking care of the households. In addition to that, I was exposed to x-rays,” she added.
 |
Dr. Kordai DeCoteau |
“When you put everything together… diet, lack of sleep, stress, work — what kind of work could you be doing that’s exposing you to this risk?” Dr. DeCoteau questioned. “Once you understand breast cancer more, hopefully you can navigate it better,” she said, adding that folks should “get tested earlier.”
Source: Asheea Smith, The Root [1/21/26]
01/21/2026
INTERNATIONAL PODIATRISTS IN THE NEWS
Aussie Podiatrist Stresses the Importance of Exercises to Keep Feet Strong
About one quarter of our bones are in our feet. How can you keep them strong and pain-free for longer? Dentists have trained us well to visit them on a regular basis for a check-up, rather than waiting until things start to hurt. Dr. Hylton Menz, a professor of podiatry at La Trobe University in Melbourne, wishes we’d do the same for our feet. “We probably ignore our feet relative to other parts of our body, because we stick them in shoes and they’re a long way away, so we tend to forget about feet,” he says. “It’s only really when they don’t actually function properly – so when they become painful, they don’t do what we want them to do – that we really think about them.”
 |
Dr. Hylton Menz |
Our entire body weight rests on the soles of our feet, so maintaining a healthy weight is an important part of looking after our feet. It’s not just for mechanical reasons but also metabolic, Menz says. “There’s really good evidence now that adipose tissue – fat tissue – is active stuff, so it tends to become activated on nerve endings, so there’s a really strong connection between foot pain and being overweight,” he says. “There’s lots of benefits to having a healthy body weight, and one of the benefits is you’re far less likely to get foot pain.” We spend so much time on our feet yet rarely think of them as a body part that needs exercising. But there are some foot exercises that can help maintain the big and small muscles in the foot that are critical for balance and movement.
Source: Head Topics [1/18/26]
01/20/2026
PODIATRISTS IN THE NEWS
NY Podiatrist Discusses Risks of Going Barefoot at the Airport
Samantha Landau, DPM, Assistant Professor of orthopedics and pediatrics at Touro University New York College of Podiatric Medicine says you should never go barefoot through airport security. First of all, there’s the risk of stepping on debris that could seriously injure you, like broken glass, sharp pieces of metal, jagged plastic that fell off someone’s overpacked rollaboard suitcase frame, or worse.
 |
Dr. Samantha Landau |
“Even a minor puncture wound can lead to infection or need medical treatment,” Dr. Landau said, adding that she once had a patient who “had been in a rush and stepped on something sharp on the floor. He didn’t notice immediately, but later developed an infection at the site. It wasn’t too severe, but it required antibiotics and a few visits to the clinic to clear up.”
Source: Michael Y. Pork, Upgraded Points [1/17/26]







